The Connection Between Eczema and Gut Health: Unraveling the Mystery
- Dr. Serena

- Aug 7, 2024
- 4 min read

Eczema, a chronic skin condition characterized by inflammation and itchiness, affects millions of people worldwide. It is very common, especially in children, but it is not normal. While traditional treatments often focus on topical solutions, emerging research suggests a link between eczema and gut health. In this article, we'll explore the intricate connection between eczema and the gut, shedding light on the role of the microbiome in managing and preventing this skin condition.
Understanding Eczema:
Eczema, also known as atopic dermatitis, is a complex condition influenced by both genetic and environmental factors. Common symptoms include red, inflamed skin, intense itching, and a tendency to develop rashes in specific areas. Traditional treatments involve moisturizers, steroids, and immunosuppressants, but recent studies highlight the importance of looking beyond the surface and into the gut for potential solutions.

The Gut-Skin Axis:
The gut-skin axis is a two-way communication system that links the health of the gastrointestinal tract to the skin. Research suggests that an imbalance in the gut microbiome, the community of microorganisms living in the digestive system, may contribute to the development and exacerbation of eczema. This suggests that eczema is not a skin problem, but a symptom. When the gut microbiome is in harmony, it plays a crucial role in regulating the immune system and maintaining overall health. However, disturbances in this delicate balance can lead to various health issues, including skin conditions like eczema.
The Microbiome's Role in Eczema:
Several studies have explored the correlation between the gut microbiome and eczema. It's been found that individuals with eczema often exhibit alterations in their gut bacteria composition. The diversity and abundance of beneficial bacteria, such as Bifidobacterium and Lactobacillus, are often reduced in those with eczema. In contrast, harmful bacteria like Staphylococcus aureus may become overrepresented.
These microbial imbalances can trigger inflammatory responses and compromise the skin barrier, making individuals more susceptible to eczema flare-ups. Understanding and addressing these imbalances may pave the way for innovative eczema treatments that go beyond the conventional topical approach.
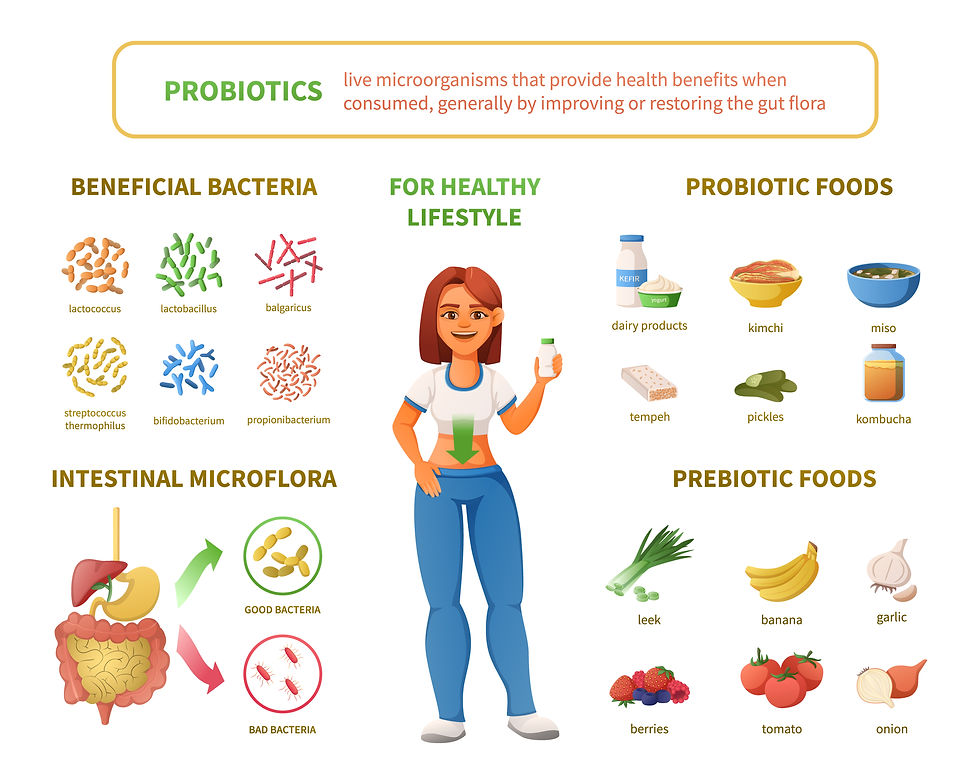
Image by macrovector on Freepik
Probiotics and Prebiotics for Eczema:
Treating eczema as a skin problem overlooks the root cause. One promising avenue for managing eczema is using probiotics and prebiotics. Probiotics are beneficial live bacteria that can positively impact the gut microbiome, while prebiotics provide the necessary nutrients for these beneficial bacteria to thrive. Incorporating probiotic-rich foods like yogurt, kefir, and fermented vegetables, and prebiotic-rich foods like bananas, onions, and garlic, may help restore gut balance and alleviate eczema symptoms.
In addition, research has shown that supplementation with specific probiotic strains, such as Lactobacillus rhamnosus and Bifidobacterium breve, can improve eczema symptoms. These findings highlight the potential of personalized microbiome interventions tailored to an individual's unique gut composition.
Gut Health and Low-Level Laser Therapy:
Red light therapy (RLT), also known as photobiomodulation (PMB) and low-level light therapy (LLLT), is an innovative biohacking technique that uses red and near-infrared (NIR) light to supercharge your cells and, as a result, boost overall health and wellness.
When red and NIR light is absorbed into the skin, it affects the body’s cellular health, improving an individual’s health and longevity from the cellular level. Research has also shown laser therapy can increase beneficial gut bacteria in just 2 weeks. Cold laser therapy has become a large alternative form of treatment due to its cost-effectiveness, ease of treatment, and no side effects to the patient. The treatment doesn’t break the skin's surface and produces no ionizing radiation so the treatment is perfectly safe.
Conclusion:
The link between eczema and gut health represents a groundbreaking frontier in dermatology. By delving into the relationship between the gut microbiome and skin conditions, researchers and healthcare professionals aim to revolutionize eczema treatment strategies. As our understanding of the gut-skin axis deepens, individuals with eczema may find relief and improved skin health through personalized approaches that address the root causes within the gut. Embracing a holistic perspective that encompasses both internal and external factors could pave the way for a new era in eczema management.
Research Articles:
Oetjen L.K., Mack M.R., Feng J., Whelan T.M., Niu H., Guo C.J., Chen S., Trier A.M., Xu A.Z., Tripathi S.V., et al. Sensory Neurons Co-opt Classical Immune Signaling
Pathways to Mediate Chronic Itch. Cell. 2017;171:217–228.e13. doi: 10.1016/j.cell.2017.08.006.
Liang Y., Chang C., Lu Q. The Genetics and Epigenetics of Atopic Dermatitis-Filaggrin and Other Polymorphisms. Clin. Rev. Allergy Immunol. 2016;51:315–328. doi: 10.1007/s12016-015-8508-5.
Zhu T.H., Zhu T.R., Tran K.A., Sivamani R.K., Shi V.Y. Epithelial Barrier Dysfunctions in Atopic Dermatitis: A Skin-Gut-Lung Model Linking Microbiome Alteration and Immune Dysregulation. Br. J. Dermatol.
Zheng D., Liwinski T., Elinav E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020;30:492–506. doi: 10.1038/s41422-020-0332-7.
Fujimura K.E., Slusher N.A., Cabana M.D., Lynch S.V. Role of the gut microbiota in defining human health. Exp. Rev. Anti-Infect. Ther. 2010;8:435–454. doi: 10.1586/eri.10.14.
Hill D.A., Artis D. Intestinal bacteria and the regulation of immune cell homeostasis. Annu. Rev. Immunol. 2010;28:623–667. doi: 10.1146/annurev-immunol-030409-101330.
Park Y.M., Lee S.Y., Kang M.J., Kim B.S., Lee M.J., Jung S.S., Yoon J.S., Cho H.J., Lee E., Yang S.I., et al. Imbalance of Gut Streptococcus, Clostridium, and Akkermansia Determines the Natural Course of Atopic Dermatitis in Infant. Allergy Asthma Immunol. Res. 2020;12:322–337. doi: 10.4168/aair.2020.12.2.322.
Watanabe S., Narisawa Y., Arase S., Okamatsu H., Ikenaga T., Tajiri Y., Kumemura M. Differences in fecal microflora between patients with atopic dermatitis and healthy control subjects. J. Allergy Clin. Immunol. 2003;111:587–591. doi: 10.1067/mai.2003.105.
Lee S.Y., Lee E., Park Y.M., Hong S.J. Microbiome in the Gut-Skin Axis in Atopic Dermatitis. Allergy Asthma Immunol. Res. 2018;10:354–362. doi: 10.4168/aair.2018.10.4.354.
Salem I., Ramser A., Isham N., Ghannoum M.A. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front. Microbiol. 2018;9:1459. doi: 10.3389/fmicb.2018.01459.
Hill C., Guarner F., Reid G., Gibson G.R., Merenstein D.J., Pot B., Morelli L., Canani R.B., Flint H.J., Salminen S., et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014;11:506–514. doi: 10.1038/nrgastro.2014.66.
Gueniche A., Benyacoub J., Philippe D., Bastien P., Kusy N., Breton L., Blum S., Castiel-Higounenc I. Lactobacillus paracasei CNCM I-2116 (ST11) inhibits substance P-induced skin inflammation and accelerates skin barrier function recovery in vitro. Eur. J. Dermatol. 2010;20:731–737.



Comments